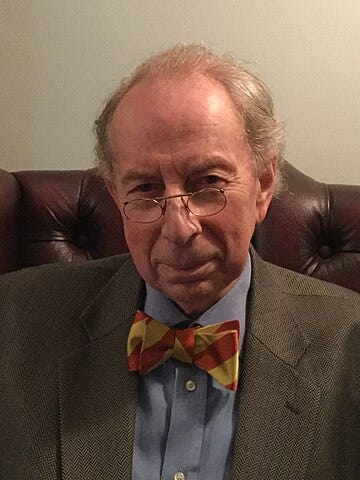
Dr. Vernon Coleman: How Doctors Killed My Mother
The following essay is taken from my book entitled `How and Why Doctors Kill More People than Cancer’
One-time or recurring donations can be made through Ko-Fi:
Part One
In October 2004 my mother had difficulty in walking. When she was first admitted to Royal Devon and Exeter hospital in Exeter, she was thought to need extensive physiotherapy to help her walk again. She was mentally alert. In November 2004, after a rapid deterioration, it was decided that my mother was suffering from terminal cancer with metastases. She was not considered healthy enough for palliative radiotherapy. She was described, by her consultant oncologist, as `frail, confused, bedbound and dependent'. She had to be catheterised because she was incontinent. The idea of rehabilitation was abandoned because of her alleged terminal cancer. A neurologist who assessed her mental state reported that my mother did not know where she was and had failed to recognise the doctor. She was given the usual simple mental test (date of birth and so on) and scored 0 out of 10. My father was telephoned at home and told that my mother was terminally ill with cancer and that there were metastatic deposits in her spine, lung and possibly liver. It was thought that her mental condition could be caused by secondaries in her brain. No one knew what sort of cancer she was suffering from or where the primary was situated. My father was telephoned and told that a breast cancer she had many years earlier, and from which she had officially recovered, had suddenly recurred, though there was absolutely no evidence for this theory. (Following an operation to remove a breast, she had refused chemotherapy and radiotherapy after asking to see evidence that the proposed treatment might be suitable for a woman of her age. Although she was over 70 at the time she was only given evidence showing that the suggested treatment might be suitable for premenopausal women. My mother, who had left school at 14, could see at a glance that this wasn't of much relevance to her. She decided that `it's what we do' didn't count as a scientific explanation and so she and my father decided that she'd pass on those, thank you very much for offering. She made a complete recovery but now, years later, as she lay in her hospital bed various members of staff blamed the cancer. My father was devastated. The diagnosis caused him untold grief, soul-searching and guilt. It subsequently turned out that the people who told him this were quite wrong. My mother's illness and her death had absolutely nothing to do with the breast cancer.
I telephoned the cancer specialist. She told me that my mother either had cancer of the breast or the lung with secondaries and was too weak for treatment. `That's the nature of the beast', she said. She told me that there was no hope but did agree that the registrar's action in telephoning my father when he was at home alone was barbaric.
On Sunday 21st November we noticed that my mother's urine bag was red. There was clearly blood in her urine. A nurse had changed the catheter bag several times without bothering to report to anyone that the urine in the bag was red with blood. Or perhaps they hadn't noticed. I reported the blood and a doctor put my mother on amoxicillin for a urinary infection. After the blood appeared in the urine the cancer specialist told me that my mother had secondaries in her kidneys. By the 30th November the urine was clear and the bag was no longer red. The diagnosis of cancer secondaries in the kidneys was never withdrawn, though it too was wrong.
My mother stayed in the Exeter hospital, which is a teaching hospital, for the next few months. Numerous consultants saw her and decided that there was nothing to be done. Her symptoms now seemed to defy diagnosis. She managed to get out of bed occasionally but was unsteady on her feet. And she had developed a rather strange way of walking with her feet wide apart.
My wife, Antoinette, who has no medical training, put my mother's symptoms into an Internet search engine. She came up with several differential diagnoses. From the short list she produced we both agreed that normal pressure hydrocephalus was the most likely diagnosis. I’d never heard of it but the disease fitted my mother's symptoms perfectly.
She had an unusual wide-legged walk. She had a tendency to fall. And she had urinary incontinence. She was also showing signs of dementia. These are precisely the symptoms shown by patients with normal pressure hydrocephalus. Precisely.
Normal pressure hydrocephalus is not something GPs see very much if ever. But it is the sort of thing teaching hospital neurologists really should know about. I had never seen a patient with it. The doctors looking after my mother listened politely to my suggestion that they consider normal pressure hydrocephalus but immediately dismissed it and stuck with their neoplastic madness. There was never a shred of evidence in support of that diagnosis.
At one point during her stay in the Exeter hospital my mother improved noticeably after she had a diagnostic lumbar puncture and some cerebrospinal fluid was removed. I thought that the improvement might be significant. It was the only time during her stay in Exeter that she showed any signs of improvement. For a day or two she seemed stronger and her mental function even began to improve a little. It seemed to me to suggest that there had been too much fluid around my mother's brain. Maybe the lumbar puncture, by removing some of the fluid, had reduced the pressure and alleviated her symptoms. Maybe the diagnosis of normal pressure hydrocephalus was correct after all. The doctors to whom I mentioned this dismissed my suggestion and insisted that the improvement was simply a coincidence. What would a former GP and writer of books know about these things? No one actually patted me on the head but it felt as though they had done so.
After my mother had finally been diagnosed as suffering from normal pressure hydrocephalus (just before she died) I checked with a large medical textbook. Here is what it says: `To help with the diagnosis, doctors do a spinal tap (lumbar puncture) to remove excess cerebrospinal fluid. If this procedure relieves symptoms, normal pressure hydrocephalus is likely, and treatment is likely to be effective.'
There are very few devastating diseases that can be cured so cheaply, so quickly and so permanently.
In the spring of 2005 my mother was still in the hospital and her condition had deteriorated. On Monday 25th April 2005 I saw the neurology registrar at the Royal Devon and Exeter hospital who confirmed that my mother's prognosis was bleak. The hospital staff still hadn't made a diagnosis. The cancer diagnosis had been forgotten. I was told that six neurologists and numerous other consultants had seen her. Every conceivable test had been done. The registrar told me that it would be difficult to find a nursing home capable of looking after her. In addition to her physical paralysis she was again diagnosed as suffering from dementia. I was told that this could be vascular or a consequence of possible encephalitis. It seemed clear that my mother needed to stay in hospital for the rest of her life.
I was advised that there were no nursing homes in Budleigh capable of looking after my mother. Afterwards we sat by my mother's beside. Antoinette, my wife, was feeding my mother. I sat on the other side of the bed. As we left my mother pulled her urine catheter bag out from under the bedclothes and tried to blow her nose with it.
On Tuesday 26th April 2005 my mother was, at my request, moved to Budleigh hospital so that my father, who lived in Budleigh, could visit more easily. For six months he had visited the Exeter hospital once or twice a day to feed my mother (who would otherwise have almost certainly starved to death). I also wanted my mother out of the hospital in Exeter because I wasn't terribly impressed by the nursing care she had received. If I had to choose two words to describe the hospital care they would be `apathetic' and `neglectful'.
On Wednesday 27th April, at 9.00 p.m., someone from Budleigh hospital telephoned my father (who is 85) and asked him when he would be moving his wife out of the hospital. This was the second time he'd received an evening telephone call that had frightened him out of his wits. My mum had been in the hospital for just slightly more than 24 hours. No one there had made any attempt to make a diagnosis. It didn't strike me as the sort of hospital that does terribly much in the way of diagnostic work. It was, it seemed to me, what used to be called a cottage hospital.
My father was startled and shocked by the suddenness and timing of the telephone call asking him when he would be moving mother out of the hospital. He got the impression that the hospital was planning to send my mum home for him to look after by himself. She was incapable of doing anything for herself. She was doubly incontinent, required nursing on a ripple bed and had been diagnosed as demented. She had to be kept in a bed with cot sides so that she didn't fall onto the floor. On the odd occasion when she tried to feed herself she ended up with food everywhere - with the result that both she and the bed had to be changed. My mother was so incapable of moving by herself that the nurses had a hoist and a bed lift fitted to the bed so that they could move my mother around and in and out of bed. It took two nurses to move her up the bed. She needed constant nursing attention.
Part Two
My wife and I were in France when my mother was moved to the hospital in Budleigh. We came straight back and visited the hospital the next day, Thursday the 28th. Within five minutes of my arriving at my mother's bedside a nurse asked me to go to the sister's office. A nurse wanted to know when my mother would be leaving the hospital. My mother had, by then, been in the hospital for no more than 48 hours. I found the questioning cruel, unfeeling and inhumane. Throughout my mother's stay I found the hospital staff aggressive and offensive.
My father, who had been in a state of shock, now became depressed as a result of the hospital’s attitude. Up until Monday the 25th April, my father had hoped that he would be able to have my mother back home or that, at the very least, he would be able to take her out of the hospital for trips in a wheelchair. He had been making plans to buy a motorised chair and a suitable vehicle so that he could do this. He thought a week or two in the hospital would lead to her returning home.
When I spoke to the nurse at Budleigh Hospital on 28th April 2005 I was told that an assessment had been done and that my mother was considered fit to move out of the hospital and was now regarded as mentally alert. My mother had, according to Budleigh Hospital, been cured from her dementia within two days. She had received no new treatment. She had merely been moved to a local small town hospital. The nurse admitted that my mother needed nursing care but insisted that mentally there was nothing wrong with her. The hospital had, she told me, already applied for an enforcement order to have my mother removed from the hospital. I was shocked by their ruthlessness.
In reality, there had been no change whatsoever in my mum’s condition. Several neurologists at Royal Devon and Exeter hospital had already agreed that my mother was suffering from severe dementia and though it turned out that they had missed the primary diagnosis there wasn't much doubt that a diagnosis of dementia was understandable - at least it would have been if it had been a diagnosis made by a nurse or a member of the public. Through a mixture of stubbornness and stupidity the highly paid hospital specialists had missed the crucial diagnosis (even though it had been handed to them on a plate) but neither we nor anyone at the Budleigh hospital knew that.
I complained about the fact that my father had been rung at home the evening before but the nurse didn't seem to think that there was anything wrong with that. She didn't apologise. I wanted to know just how ill you had to be to be in hospital these days. I felt overwhelmed with guilt. I had arranged for my mother to be moved to the Budleigh Hospital so that my father could visit more easily. And now they wanted to throw her out. But where could we take her? I went back to sit by mother's bed. As I sat down my mother looked up and pointed to a stranger on the other side of the ward. `Is that Vernon over there?' she enquired. We were living a nightmare. She didn't know who I was. She didn't recognise my wife. And she often wasn't sure who my father was. When I talked to her she didn't even know that she was in hospital. Somewhere in the hospital a bell rang. `There's someone at the door,' she said.
Someone at the Budleigh hospital threatened to send my mother home in an ambulance, even though they knew that my father could hardly look after himself. They also knew that my mother needed intensive nursing care. My mother was, said one snotty little bastard, terminally but not finally terminally ill. It was the first time I'd heard the phrase. My father, in his mid 80s, was devastated. `What do I do if they send her home?' he asked. `Don't answer the door,' I told him. `Don't let them into the house. Call me.' I was telling my father to refuse to let the ambulance men bring my mother into the house. It was awful, just bloody awful. If the plan was to put us under pressure it was working very well. I'd never seen my father so distraught. My mother's GP at the time, Dr Taylor, agreed that we would not be able to find a local nursing home capable of looking after her. No one at the Budleigh hospital seemed to me to give a damn what happened to my mother as long as she wasn't their responsibility.
As far as I am aware no one made the slightest attempt to make a diagnosis during the time my mother was in the Budleigh Hospital. Since they didn't want to nurse her and they didn't do any diagnostic tests it's difficult to see the point of the hospital - apart from providing employment for the staff.
On the 11th May I had to attend a meeting at Budleigh hospital to discuss my mother's expulsion from the hospital. I was told that the hospital did not have enough beds and desperately needed to get rid of my mother. There were four people at the meeting: two members of the nursing staff, someone who looked like an administrator and Dr Taylor, my mother's GP at the time. I mistakenly thought that he at least would be on my parents' side. I was disappointed. The meeting was held in a completely empty ward. There were plenty of beds, all empty, and it seemed to me that this wasn't the first time the empty ward had been used for a meeting. If the hospital was short of anything it was patients, not beds.
The meeting lasted an hour and it turned out to be one of the most unpleasant hours of my life. I have been grilled by some of the country's toughest television and radio interviewers. I have given evidence in the House of Lords and the House of Commons but nothing prepared me for this. For a solid hour the four of them battered at me to take my mother out of the hospital. They used every manipulative and emotional trick in the book. I quickly realised that no one there cared a damn about my mother or my father. They just wanted to get rid of a patient who seemed likely to be a long-term expense. This was business. I was still desperate to try to find a diagnosis. I was still trying to support my father. I was grieving for my mother who no longer even recognised me. I was told that my mother would be better off in a nursing home and that the hospital didn't have any long-stay beds. I was told that they needed the bed for other patients (no one seemed to see the irony in the fact that the meeting was being held in a completely empty ward) and that my father would be better off if my mother was elsewhere. They didn't explain how this could be when there was no nursing home for miles that would be able to cope with her needs. My father lived near to the hospital and could easily visit within minutes. I was told that my mother would be better off in a private room. I pointed out that she couldn't read or watch television or listen to the radio. She had no memory or mental capacity. I pointed out that being in a hospital ward gave her things to watch. I knew that being in a small, closed room would be awful for her. No one seemed to give a damn. I was told that my mother was more at risk of catching an infection in a hospital (the only thing I agreed with). At the end of the meeting they told me that they couldn't agree to my mother staying in the hospital and that she had to leave. I left the meeting and went back to my mother's bedside. She was still unable to move. She still didn't know who she was or where she was. She didn't know who I was. She was still faecally incontinent. She still had a catheter in her bladder to collect her urine. She still had to be fed. She still couldn't walk or even wash herself. But according to the hospital staff she was fine and mentally alert. I wondered if they wanted to throw my mother out because they knew we could afford the nursing home fees. Ageism is the new racism: no respect, no consideration, no courtesy, no dignity, no caring. The whole penny pinching exercise was made even more heartless and unforgivable by the fact that I know that hospital staff waste billions through incompetence. Billions are stolen and frittered away by the wicked statist guardians we pay to look after us.
For several weeks after that my father didn't dare visit my mother at all. He was frightened that he would again be pressured by the staff to move my mother. He didn't know where he could take her. He was overwhelmed with grief and now he was tortured by guilt and anxiety.
Another mental assessment was done on my mother. It was a sick joke. The assessor asked my mother what I did for a living. My mother thought for a while. `He's a teacher,' she said at last. She didn't know who I was, let alone what I did for a living. `That's close enough,' answered the assessor putting a tick in another box. My mother was declared mentally competent. On the 19th July my mother complained to me that two dogs had been fighting on the ward. On the 22nd July my father was sitting by my mother's side when the vicar called. My mother told him they were waiting for a train. The vicar thought it was a joke but my mother was serious. She kept asking my father why the train wasn't there. My mother didn't recognise my father or know what he'd done for a living. She didn't know anything. She didn't even know who she was or where she was. She held her head a good deal though and it was clear that she was having constant headaches. (No one at the hospital realised that these were caused by the increase in the amount of fluid surrounding her brain.)
On the 27th July I attended another meeting in Budleigh Hospital. This time there were nine people there representing the hospital and the NHS. Nine of them. Dr Graham Taylor, my mother's GP was there, together with two nurses, a ‘continuity care manager’, an ‘acting leading continuity nurse’, a ‘hospital care manager’, a ‘discharge facilitator’, a representative of the administrators and a representative from Exmouth social services. I wrote down all their names. Someone began by saying that they all had my mother's best interests at heart. Someone else said they were delighted to report that my mother was much better and was improving. I asked them why, if this was the case, they weren't giving her any occupational therapy or physiotherapy. No one had an answer to this. I got the impression they thought it was an unfair question. I asked them how they had managed to produce this miracle without any treatment. I wanted to know how a woman who had been officially declared terminally ill and demented and in need of constant care had suddenly become `physically capable and mentally alert' after a few weeks in a small town hospital. No one had any answers. In fact, of course, when the final diagnosis was made it was quite clear that my mother could not possibly have shown any physical or mental improvement. She was suffering from normal pressure hydrocephalus which was steadily getting worse. And very early on in the illness she had been officially declared to be demented.
The hospital staff who said that she had recovered and could be discharged were completely wrong. I find it difficult to avoid the suspicion that they said she was better simply because they wanted to throw my mother out of the hospital. Bizarrely, the continuity care manager wanted proof that I represented my mother and made what he called a formal objection to the fact that I had not given them my home address. When I pointed out that my mother needed intensive nursing care he claimed, to my utter astonishment, that catheters, hoists and ripple beds were not medical equipment. I asked him what would count as medical equipment. He said a ventilator would count as medical equipment. So, presumably, if my mother had been on a ventilator they wouldn't have wanted to throw her out. One of the `nine' said that they only paid for the care of patients who were in the final stage of cancer. The phrase `final stage terminally illness' was used. And again I heard the phrase `terminally, terminally ill'. I asked how they knew that a patient was terminally, terminally ill and was told that they could tell this through liver and kidney deterioration. I asked if they had done any tests to check on this and it was generally agreed that they couldn't remember whether any such tests had been done. I got the impression they seemed to think the question was embarrassing and therefore unfair. I have no idea why nine people wasted a good chunk of a day on such a pointless meeting. I hate to think what it must have cost. It occurred to me as I sat there that if they were all sacked there would be plenty of money left for looking after patients and I told them that the bullying had won and that we would take my mother out of the hospital so that they could have yet another empty bed. I don't think I ever saw any of the nine again.
According to the law the NHS had a full responsibility for looking after my mother. According to the relevant legislation the NHS was expected to arrange and fund rehabilitation and recovery services and palliative care. It is inconceivable that my mother did not fulfil the eligibility criteria for continuing NHS healthcare. The law is clear: if the primary need for care is due to severe ill health, then all costs of nursing, personal care and accommodation should be funded by the State health service. Today, on reflection, it seems to me that the nine people at the meeting at Budleigh Hospital had become institutionalised and were working for the system and not for patients.
In the end my father couldn't bear it any longer. I really couldn't blame him. The staff at the Budleigh Hospital were making us feel so unwelcome, and harassing us so much, that we had no choice but to move my mother. As far as the NHS was concerned it was all about money. They wanted to avoid the cost of looking after my mother - even though they had a moral and legal responsibility to do so. My father, my wife and I all knew that moving my mother out of the hospital was the wrong thing to do for her because she needed the hospital environment but in the end my father just couldn't cope with the pressure. I don't blame him. We found the Cranford Nursing Home, a private nursing home in Exmouth, which could cope. For around £750 a week my mother had a private room which seemed crowded with three adults visiting. My wife and felt that the en suite `bathroom' was more like a cupboard and we both felt that if a hotel had offered us the room we would have walked out in disgust.
My father sold his home and bought a small house near to the nursing home so that he could visit regularly. My mother was tearful when she moved into the nursing home. She had hardly spoken for months. But she spoke now. The first thing she said was: `I don't like it here.' Because much of their money was in joint accounts, and my mother couldn't sign her name, my father had to arrange for a power of attorney so that he could access their savings and pay the nursing home fees. (Even this was not always accepted, and my dad had no choice but to forge my mum’s signature.)
My mother died in the nursing home. The diagnosis had by then been made. Numerous consultants (including several neurologists), countless junior hospital doctors, one or two GPs and a good many nurses all missed the diagnosis. (Since nurses now want to be regarded as almost equal to doctors they must take some of the blame). We watched my mother die a terrible, slow death. She died because the doctors failed to make the diagnosis until it was too late.
Towards the end of her life we visited my mother in the nursing home and as soon as Antoinette entered the room she turned to me and said that my mother had a swollen, bulging eye. The diagnosis now was beyond doubt. My mother had a bulging eye because of the pressure inside her skull. I contacted my mother's new GP and asked him to arrange for my mum to go back into Exeter hospital. I don’t think he or any of the people looking after my mother in the nursing home had realised the significance of this. In the Royal Devon and Exeter Hospital the doctors at last confirmed the diagnosis of normal pressure hydrocephalus. It was the diagnosis we'd offered them within a month of my mother falling ill. It had taken endless NHS doctors and two NHS hospitals to reach the diagnosis. If they'd acted within days or even weeks of her being admitted then they could have saved her life. Treatment for normal pressure hydrocephalus is easy, fast, cheap and effective. A shunt is placed in the ventricles of the brain and run under the skin. Cerebrospinal fluid is then drained away from the brain. This procedure will then significantly improve the symptoms.
But by now it was too late. On the death certificate my mother's death is recorded as dementia with normal pressure hydrocephalus as the underlying problem. I never told my dad how my mother could have been saved. It was, for my mother, a slow and painful and humiliating death. If it can happen to my family it can happen to yours. Remember, it is only because I am a doctor (and my wife is an excellent researcher) that we finally managed to persuade the doctors to (belatedly) reach the correct diagnosis. Remember that in order to save money NHS staff in Budleigh insisted that my mother was rational and mentally alert (when she was suffering from dementia). Remember, too that we failed to save my mother's life. She was killed by incompetence. No one has ever apologised. No one has ever admitted that any mistakes were made. And I have no doubt that no one ever will.
The above shortened essay is taken from the book `Why and how doctors kill more people than cancer’ by Vernon Coleman. To purchase a copy CLICK HERE
Copyright Vernon Coleman August 2024
Related articles:














God, what a sad, sad story. It's like we all have to become our own researchers and doctors. We are all aging and will most likely need hospital care later (assuming you are not receiving now). Are there any good diagnostic/AI tools where you just enter the symptoms and it spits out all possible causes and each probability?
I am sorry for your loss. I tell my patients daily, ‘that if you go to the hospital, they will kill you. So let’s do what we can, at home, to stay out of their care.’